
Queen Latifah calls for more ‘inclusive healthcare’ for people with obesity
Queen Latifah is calling for more inclusive medical care for people with obesity. In a new interview as part of her work with It’s Bigger Than Me, a US-based campaign by healthcare company Novo Nordisk, the actor and rapper recounted how many people with obesity experience weight discrimination from medical staff. Sharing her personal connection to the issue, the Girls Trip star – whose real name Dana Owens – toldPeople: “I saw my cousin have to deal with this issue – she was morbidly obese and she went in and out of the hospital. “There were so many things she had to face. And for a doctor to just say, ‘Oh, you need to lose some weight.’ Well, it’s not that easy. Everyone’s bodies are not the same. We all deserve specific individual care.” Latifah, 53, backed the campaign’s call for “inclusive obesity care” ensuring everyone can feel “welcome and respected” when they visit the doctors. “Imagine how good it must feel when a patient walks through that door and sees the appropriate chairs or office set-up, that someone has considered them, has taken the time to think about what their needs are,” the Hairspray star said. “There’s a sense of, ‘I’m respected here. I’m welcome here’... If you’re discouraged to get into your doctor’s office, then that’s not a good thing.” When a person is defined as obese, this means that they are overweight “with a lot of body fat”, the NHS says. The World Health Organisation (WHO) explains that the terms “overweight” and “obesity” are used to refer to “abnormal or excessive fat accumulation that presents a risk to health”. It is estimated 64 per cent of adults in the UK are obese or overweight. Last summer, a British study found that obese patients were being “weight-shamed by doctors and nurses”, with weight stigmatisation pushing patients to skip appointments. The stigmatisation leads to patients avoiding appointments, feeling depressed or anxious and being more likely to put on weight, scientists said. The British researchers said there needed to be better education for medics over “weight stigma” to avoid this spilling into healthcare. The scientists looked at more than 3,000 research articles on the topic to identify strategies to tackle negative biases towards overweight and obese patients. In doing so, this could help to tackle the UK’s obesity crisis, as negative biases over weight limit access to healthcare services and treatment. Read More Joe Wicks defends decision to pull five-year-old daughter out of school Woman adopts husband’s ex-wife’s son after growing up in foster care herself Man who went to Turkey to make himself taller says pain was ‘worth it’ As Simon Cowell shares positive therapy experience, how can it help even if you aren’t in crisis? Man who went to Turkey to make himself taller says pain was ‘worth it’ Terminally ill mum prepares for worst after numb hand turns out to be deadly disease
2023-08-31 22:16

Kylie Jenner Considers Buying Back Coty’s $600 Million Stake in Her Makeup Brand
Kylie Jenner has explored taking back ownership of the cosmetics line she sold to Coty Inc. three years
2023-08-31 21:57

Women Basketball Players Have Been Stuck Playing in Men’s Shoes
For Courtney Williams, a guard for the WNBA’s Chicago Sky, breaking in her shoes to get them to
2023-08-31 21:55
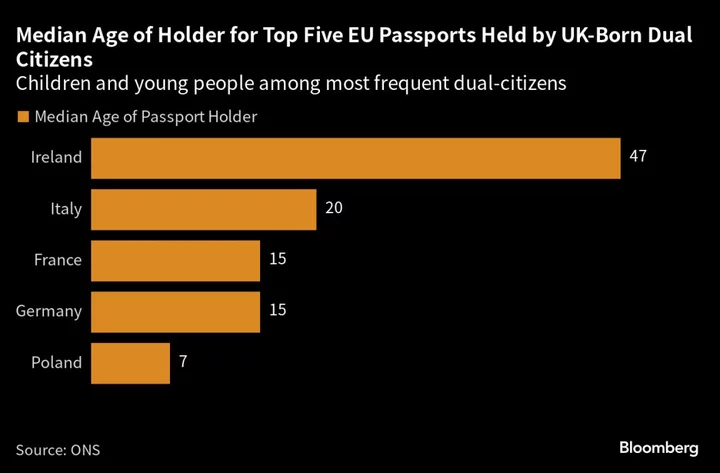
UK Census Shows Dual Citizenship Numbers Doubled Since Brexit
The UK said the number of residents in England and Wales with dual citizenship doubled in the decade
2023-08-31 21:51

Campbell Soup sees upbeat annual profit on easing costs, snack demand
By Deborah Mary Sophia Campbell Soup forecast annual profit largely above Wall Street estimates on Thursday, encouraged by
2023-08-31 21:51
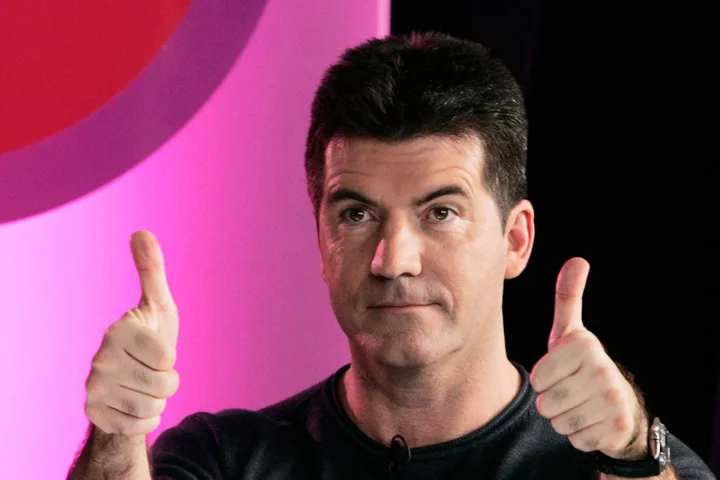
As Simon Cowell shares positive therapy experience, how can it help even if you aren’t in crisis?
X Factor boss Simon Cowell, 63, has shared that having discovered therapy in the past year, he feels as though “a weight has lifted off my shoulders”. The music mogul, who is behind The X Factor and Britain’s Got Talent, said he wished he had seen a therapist “10 or 20 years ago” in a recent interview with the Daily Mirror. He also shared that the deaths of his parents and the coronavirus pandemic had affected his mental health. Seeking therapy has been transformative for Cowell and it could do the same for you, whether you are in crisis, or just want to learn more about yourself. Cowell has said engaging in therapy had a “super positive effect” on his life and encouraged others to do the same, so here’s what you should know. There are different types of therapy Contrary to what many people may believe, counselling, where you sit and talk through events and reflect, is not the only form of therapy. “There are a whole host of different types of therapies available, from counselling, cognitive behavioural therapy, mindfulness-based cognitive therapy, acceptance and commitment therapy, interpersonal therapy, psychodynamic psychotherapy to eye movement desensitization and reprocessing,” explains psychologist and author of The Self-Care Revolution, Suzy Reading.Each one can have a different role in helping you get to know yourself better, handling trauma, feeling more grounded and coping more day-to-day. Therapy isn’t just for rock bottom Therapy doesn’t have to be a last resort. “When it comes to therapy, there are no hard and fast rules,” says Liz Ritchie, a St Andrew’s Healthcare psychotherapist. “Many people associate seeking help with crisis, but there is no reason why you cannot maintain regular sessions with your therapist. There is now a wealth of evidence that supports that therapy can also be a preventative form of mental healthcare, a little bit like going to a dentist or a doctor. “Life is busy and stressful, which means we don’t often have time to process cross words with a loved one, work altercations or issues with friends and family members.” You’ll understand yourself better You may think you understand yourself totally, but there are always new parts of ourselves to get to know. “Therapy helps us better understand ourselves, our relationships and the world, connecting us with how we feel, and why we might feel as we do. It is a journey of self-discovery, helping us appreciate our strengths and identify our values,” says Reading. It could give you an emotional toolkitIt can be helpful to have “an impartial sounding board to speak openly and honestly and the opportunity to be heard, validated and understood”, says Reading. “Therapy helps us challenge unhelpful thoughts, dispute self-limiting beliefs and can help us create new habits. Therapy is also about developing healthy ways to move through our emotions, creating a fresh toolkit of coping strategies and can be very practical in nature by helping us address specific challenges or goals.” But… it isn’t easy Unfortunately getting therapy is not always easy. If you do not have the financial freedom to be able to pay for a private therapist, you may be faced with long waiting lists and restrictive services. However, NHS therapy is an option and can be really helpful, so be sure to look into the options you can afford near you. Reading recommends checking out BPS and HCPC to find a qualified therapist. NHS resources can be accessed here. If you are seriously struggling with your mental health, and are at risk, please call 999 or the Samaritans on 116 123.
2023-08-31 20:51

Trader Joe's issues its sixth recall in two months
Trader Joe's has issued another food recall — its sixth since July.
2023-08-31 20:46

Alabama attorney general says he has right to prosecute people who facilitate travel for out-of-state abortions
Alabama's Republican attorney general said in a court filing that he has the right to prosecute people who make travel arrangements for pregnant women to have out-of-state abortions.
2023-08-31 19:49

Terminally ill mum wants ‘happy memories’ with family after hand numbness turned out to be deadly disease
A mum who was told she likely suffered from carpal tunnel syndrome after feeling numbness in her right hand during her pregnancy has been given just a few years to live after scans revealed she will soon be paralysed. Charlotte Parker, 28, from West Berkshire, was diagnosed with amyotrophic lateral sclerosis (ALS) nine months after giving birth and is now trying to create “happy memories” with her young family while there is still time. The rare condition, a type of motor neurone disease (MND), means Charlotte only has two to five years’ life expectancy during which time she will become increasingly paralysed. Charlotte, who lives in Thatcham with her fiance George, 32, a mechanic, and their three children, says she wants her 11-month-old son Jimmy to know she was there. Her friends and family are fundraising so she can afford to take her family to Disneyland in Paris and take advantage of what time they have left together. “I don’t think you can imagine having to tell your parents at 28 that you have been diagnosed with a terminal illness,” Charlotte, who works as a revenue and debt accountant at an energy company, told PA Real Life. “At the moment my life is so fast paced that I don’t really have much time to slow down and think about what’s happening. “Most people think MND-ALS affects older people but it actually affects a wide range of people. It can happen to anyone.” Charlotte was seven months’ pregnant when she began feeling a strange “numbness and weakness” in her right hand. “I was struggling to open jars and bottles,” she said. “Gradually it just got worse and worse and by the time I gave birth to Jimmy, I was considerably weaker. “Doing day-to-day tasks while trying to learn how to look after a newborn baby was definitely a challenge.” After flagging the numbness to her midwife, Charlotte was told she likely suffered from carpal tunnel syndrome, a common health condition caused by pressure on a nerve in the wrist. But Charlotte was referred to a neurologist when she went for a routine checkup six weeks after Jimmy was born. “He sent me for an MRI in January for possible inflammation in the brain,” she said. “I think subconsciously at the time that’s when I knew it was something a bit more serious.” While Charlotte was worried, her results came back and suggested there was no problem with her brain or spinal cord. Instead of getting better, however, the numbness started to spread to her other hand. “I kept calling because it started going into my left hand as well,” she said. “I am still able to move my fingers in my left hand but my right hand does not really work anymore.” In June, Charlotte was given an electromyography, a medical test which looks at how a person’s nerves and muscles respond to stimulation. “They put stickers on you and send pulses up your arm,” she said. “I got called in to see the neurologist quite quickly after that, which is when he advised that he strongly believed that it was MND-ALS.” I want to do as many days out with the children as possible so that we have those memories all together. Charlotte Parker ALS, the most common motor neurone disease, is incurable and causes progressive weakness and paralysis, usually leading to death within three to five years, the National Institute of Neurological Disorders and Stroke said. Charlotte’s worst fears were confirmed after she visited John Radcliffe Hospital in Oxford in July and was formally diagnosed. “It’s been a lot to adjust to, especially with a four(-year-old), seven(-year old) and eleven-month-old,” she said. “To know that there is no cure or treatment that will give me a substantial lease of life. “It is just going to deteriorate pretty quickly.” Charlotte broke the devastating news to her family and friends that her illness is terminal. “My youngest is completely none the wiser and the girls are aware that my hands are getting weaker and that it will move to my legs, but we haven’t gone into the detail of what it means will happen.” Unfortunately, doctors are unable to say how quickly Charlotte’s condition is progressing. “Each person’s story is different,” she said. “It’s such a maze on how one person’s body deteriorates to the next.” But Charlotte is not letting the diagnosis get in the way of her family plans. The mum, who does not have life insurance, plans on continuing to work for “as long as possible”. “I am fortunate that my work provides death in service,” she said. “If I can, I will try and work for as long as possible so that my partner and children do have something to help them for the next however many years.” She also plans on marrying the “love of her life”, George, after getting engaged two years ago and falling pregnant. “I fell pregnant and it just got pushed to the side. I didn’t want to get married nine months’ pregnant,” she said. “It’s time for us to celebrate us as a couple rather than just accepting that we’re not going to be together for the rest of our lives. “We have to make good of what we can and celebrate what we do have, right now, rather than just accepting the situation.” The couple, who recently went on holiday to Pembrokeshire, are also looking to create “happy memories” while there is still time. “We were on the beach late evening, when it was raining and full of wind, and we were taking photos running in and out of the sea to make memories,” she said. “I want to do as many days out with the children as possible so that we have those memories all together. “Even silly things, like being there for Jimmy’s first haircut and taking him to feed the ducks so that we can capture those memories and that he knows that I was there.” Charlotte’s friends have set up a fundraiser on GoFundMe to help them cover their costs, including a trip to Disneyland, Paris. “It would be a great trip to have with them,” she said. “I just want to enjoy my family and do as much as I can with them because there will come a point where even though I’m around, it will be a lot more complicated.” They have so far raised £11,235 of their £15,000 target. Charlotte continued: “A huge thank you to anyone who can help and it will go to creating some of the best memories I can with my family before the inevitable does happen.” To support Charlotte, visit: www.gofundme.com/f/complete-her-wishes-with-her-family Read More Woman’s blood cancer misdiagnosed as carpal tunnel due to burning hand pain What happens to your brain when you’re pregnant? Cyclist completes 960-mile ride to remember friends who died from MND What is sickle cell disease and how do you know if you have it? Project launched to bust myth that cancer is a ‘white person’s disease’ Man who lengthened his limbs by three inches says he feels ‘so much happier’
2023-08-31 17:53

Project launched to bust myth that cancer is a ‘white person’s disease’
More must be done to get black, Asian and ethnic minority people to participate in breast cancer trials, experts have said, as they warned that people from these backgrounds have been under-represented in previous studies. Medics said that they want research into the disease to be “relevant to people we see in the clinic”. Experts said that there is a “broad misperception” that black women “don’t suffer as much from breast cancer” which can result in the perception that “cancer is a white person’s disease”. If I hadn’t gone on the trial at The Christie, I wouldn’t be here today Jasmin David This is despite the fact that previous studies have found that black women are more likely to die from breast cancer compared to their white peers. They are also more likely to develop more aggressive cancer and be diagnosed when their cancer is at a more advanced stage. It comes as the NHS Race and Health Observatory launched a new campaign alongside Macmillan Cancer Support to improve diversity in breast cancer clinical trials. The project, which is being supported by Roche, aims to raise awareness of the lack of diversity in clinical studies, improve communications and provide longer term support to patients. Specialist nurses will be provided at two major cancer hubs – Bart’s Health NHS Trust in London and The Christie NHS Foundation Trust in Manchester – to help guide patients through the process. Men, who account for 1% of breast cancer patients in the UK, are also being included. The NHS Race and Health Observatory said that there are “multiple barriers” around the recruitment, communication and retention of black, Asian and ethnic minority patients in clinical trials. It said that data show that people from an ethnic minority background are poorly under-represented in many clinical trials. And the Caribbean African Health Network said that there has been a “disengagement” in research “as a result of mistrust”. Jasmin David, a 53-year-old breast cancer patient from Fallowfield in south Manchester, took part in a clinical trial which saved her life and is encouraging others to do the same. Two years after her initial diagnosis and treatment at The Christie she was told that the cancer had come back and had spread to her lungs, lymph nodes and chest bone. The mother-of-two was told she had less than a year to live but was also offered the opportunity to take part in a clinical trial at the National Institute for Health and Care Research Manchester Clinical Research Facility. Ms David is now cancer-free. “If I hadn’t gone on the trial at The Christie, I wouldn’t be here today,” she said. “I have two children and now I get to be there for them as they grow up. “Research gave me a second chance and life and I’m relishing every second of it. “I want everyone, no matter their ethnicity, to have equal access to clinical trials, so I’m glad that this important piece of work is being done. I hope that by sharing my story I can inspire more women like me to come forward and take part in clinical trials.” Dr Habib Naqvi, chief executive of the NHS Race and Health Observatory, said: “We are pleased to announce this partnership and our joint commitment to ensuring inclusion and representation in future breast cancer trials. “We believe that when targeted, culturally sensitive interventions and communications are put in place, under-represented groups can be successfully recruited into clinical trials.” He added: “There is a broad misperception that black women don’t suffer as much from breast cancer or it does not run in their family history. This can result in the perception that cancer is a white person’s disease. “We want this pilot to encourage women at risk, those already diagnosed and individuals undergoing post treatment to come forward and share their experiences and get the information needed.” Professor Richard Simcock, chief medical officer at Macmillan Cancer Support, added: “As a Breast Cancer Oncologist I want to know that research is relevant to the people we see in clinic. Historically that has not been the case. “I’m delighted that Macmillan can support this project to ensure that future evidence from clinical trials is representative and inclusive.” Charles Kwaku-Odoi, chief executive of the Caribbean African Health Network, said: “Across the black community there is an undoubted legacy of disengagement in research and most certainly clinical trials that stems back decades as a result of mistrust. “This has not served us well because it leads to a lack of appropriate interventions that perpetuate the grave health inequalities in breast cancer care. “This partnership approach to build solutions to improve engagement in clinical trials in breast cancer treatment and care is very much welcomed. We are looking forward to working in a collaborative way to build trust, improve awareness and ensure that barriers surrounding access to clinical trials are addressed.” Read More Charity boss speaks out over ‘traumatic’ encounter with royal aide Ukraine war’s heaviest fight rages in east - follow live 10 slick ways to kit out your student digs 4 essential officecore trends to update your work wardrobe Sickle Cell Awareness Month: What is sickle cell disease and how do you know if you have it?
2023-08-31 17:25

Man who lengthened his limbs by three inches feels ‘so much happier’
A Canadian man has had limb-lengthening surgery, costing £25,000, to increase his height from 5ft 7in to 5ft 10in as he was so insecure about his height it caused him to have “suicidal thoughts”, and claims he is now “so much happier” and “confident”. Daniel Farbod, 27, a civil engineer, from Toronto, Canada, has been self-conscious of his height “all (his) life” – when he stopped growing, at age 14, he said it felt “tragic” and like his “first stab to the heart.” Daniel always defined “being masculine” as being tall, and was “ashamed” of himself as he “didn’t feel like a man.” Over time, being taller was all Daniel could dream about, and claimed his height “impacted his mental health so badly” that he was having “suicidal thoughts”. After coming across the unique surgery online, he realised he was “willing to sacrifice time and money to get (his) life back.” So, in May 2021, he had his first procedure in a specialist clinic in Turkey, which involved breaking his femurs, hollowing out the bone, and putting a rod inside the bone with external fixators, pieces of steel on the outside of his legs. Daniel had to turn the fixators with an Allen key every day for over four months, and eventually had his second surgery to remove the fixators after his bones had successfully fused together. When Daniel recovered, he could not “put into words how happy (he) was” and “felt so much more confident”, now, he is sharing his journey on social media to inspire others who are insecure about their height. Daniel told PA Real Life: “I’m really proud of myself for having the surgery. “I was insecure all my life about my height, it impacted my mental health so badly. “I was suicidal, and after admitting that I wanted to take the steps to feel better, and have the surgery, I feel so much better. “I think for other people, it is important to know how tough the surgery and recovery is – it was the hardest thing I’ve ever done, but for me, it changed my life and made me grow not only literally but also metaphorically as a person.” Daniel, who has always been self-conscious about his height, stopped growing at age 14, and became obsessed with finding ways to become taller. He said: “I researched everything from socks and supplements that claimed to increase your height. “I was always insecure and worried about it – I used to go to orthopaedic doctors because I was so scared of not growing. “But when I got to age 14, I stopped and it was so depressing.” When it became clear to Daniel that he was unlikely to grow any more, it took a toll on his mental health and confidence. He explained: “It was so tragic for me, it was like my first stab to the heart. “All my dreams would be about being taller and I had to somehow accept that my height had peaked. “I tried to keep myself busy to manage my thoughts but in 2020 I just couldn’t handle it – I had all of these negative thoughts and suicidal thoughts because I think being masculine, and being a man, means to be tall. “I didn’t feel like a man, I was so ashamed.” Daniel felt as though having limb-lengthening surgery was the only way he was going to feel better, but his parents, who are both “on the shorter side”, did not approve of his decision to have cosmetic surgery. He said: “Everyone was really against the idea because they thought it was not natural and it was changing the way your body is meant to be. “I knew the surgery was going to be tough, but I thought even that pain would be better than having suicidal thoughts. “I was willing to sacrifice time and money to get my life back.” In May 2021, Daniel had his first surgery in a specialist clinic, Live Life Taller, in Turkey, which involved breaking both of his femurs, hollowing out the bone, and putting a rod inside the bone with external fixators – pieces of steel on the outside of his legs. He explained: “I was really scared when I got to the clinic, and the breaking of the bones was the part I was most nervous about in the whole process. “It was crazy to wake up after the surgery – the reality just hit me all at once and I was so happy.” His recovery involved being in a wheelchair and using an Allen key to turn a bolt on the fixators four times a day at 90 degrees to separate the bone segments a little at a time. Daniel continued to do this every day for four and a half months, saying of his painful recovery: “My skin was stretching, my muscles were growing, it was madness. “It took me even longer to recover, they usually say it will take three months, but, my I had nerve issues with my right leg and had to have it broken again. “It was a very tough time.” In September 2021, the external fixators were removed, he explained: “I used a walker and really really slowly I worked up to using crutches. “I couldn’t really tell how tall I was at that point. “It took me at least another three months to be able to stand up.” Mr Farbod went from 5 ft 7 to 5ft 10 and thinks his mental health has dramatically improved as a result. He said: “I couldn’t believe it. I had been dreaming of being a tall man since I was 10 years old, it’s all I’ve ever wanted. “I went through all these sleepless nights, trauma and upset, and I finally achieved my goal. “I can’t even put into words how happy I was, and still am – I felt so much more confident.” When Mr Farbod arrived home, his family were also very happy for him. He said: “They looked after me so much – I could barely get out of bed or bend down for a long time. “They could tell I was so much happier when I recovered.” Now, Daniel shares his journey on Instagram and YouTube to inspire others who are insecure about their height. He said: “I want to show people the reality of the surgery – it’s tough but I want to raise awareness and get men talking about their insecurities.” For support, contact the Samaritans on 116 123, email them at jo@samaritans.org, or visit samaritans.org to find your nearest branch. Read More Charity boss speaks out over ‘traumatic’ encounter with royal aide Ukraine war’s heaviest fight rages in east - follow live 10 slick ways to kit out your student digs 4 essential officecore trends to update your work wardrobe Sickle Cell Awareness Month: What is sickle cell disease and how do you know if you have it?
2023-08-31 16:48

Sickle Cell Awareness Month: What is sickle cell disease and how do you know if you have it?
Almost 300 babies are born in the UK with sickle cells every year, according to the Sickle Cell Society, and the effects of sickle cell disease are believed to impact thousands. Yet, many people may not even know what sickle cells are or what living with the condition means. What is sickle cell disease? In most people, red blood cells are disc shaped and move easily through the blood vessels. But if you have sickle cell disease, your red blood cells are shaped like a sickle (similar to a crescent moon). This stops them moving with ease through the body and blood flow becomes restricted. Sickle cell disease isn’t actually one specific disease – it refers to a group of conditions affecting people with sickle cells, which range in severity.The conditions are inherited and predominantly affect people from African and Caribbean family backgrounds. What are the symptoms of sickle cell disease? Symptoms begin early in childhood and can sometimes be debilitating. How each individual is affected may vary, but the main symptoms are anaemia, an increased risk of infections, and pain. This includes extremely painful episodes called ‘sickle cell crisis’, which happens when blood flow to certain parts of the body become blocked. According to the NHS, these episodes can last for days and require hospitalisation. Other issues are associated with the condition too, including problems with the lungs, delayed growth in childhood, higher risk of stroke, leg ulcers and sight/vision problems.How is it diagnosed? Sickle cell disease is usually picked up during pregnancy or shortly after birth, although a blood test can be given at any time to see if someone has the condition or carries sickle cell genes. In parts of the country, pregnant people will be offered a test to see what the chances are of their child having sickle cells. Infants can be checked for the cells through a heel prick test.How do you treat it? Treating sickle cell disease is usually a lifelong process to help people with pain and to stay as healthy as possible. Treatment takes place in specific sickle cell centres and those living with it are encouraged to take care of their health, no matter the severity of their symptoms. Managing pain is a huge part of treating sickle cell disease. Staying hydrated can be helpful, as well as avoiding sudden temperature changes, like getting into a cold shower or diving into water. According to the NHS, Hydroxycarbamide (hydroxyurea) may be recommended, which is taken as a pill once a day. This can lower the quantity of other blood cells and requires careful monitoring, however. Some people may also be able to have a medicine called crizanlizumab, either on its own or alongside hydroxycarbamide, usually injected into a vein every four weeks. To prevent infections, many people with sickle cell disease will take daily antibiotics. Read More Charity boss speaks out over ‘traumatic’ encounter with royal aide Ukraine war’s heaviest fight rages in east - follow live TikTok has gone wild for adult gymnastics – here’s what you should know Man explains why he swapped veganism for raw meat diet: ‘I feel great’ Rugby star Ugo Monye: Boarding school shaped my career and my personality
2023-08-31 14:49
